Understanding Dental Ozone Therapy
Dental ozone therapy can help you keep your teeth and gums as healthy as possible. So what is ozone? And what can this kind of therapy do for you? We have the answers you need.
 What Is Ozone?
What Is Ozone?
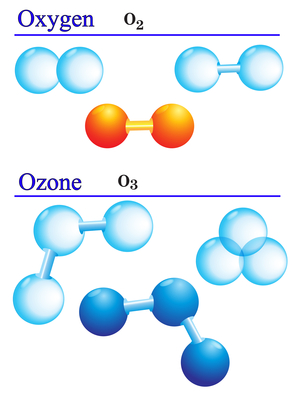
Put in the simplest way possible, ozone is three atoms of oxygen joined together in a compound. This elemental form of oxygen occurs naturally and results from lightning or ultraviolet energy, among other things. In a dental clinic, we can use an ozone generator to simulate the effect of lightning and create ozone. It’s the same substance that’s in the partially depleted layer of ozone more than 50,000 feet above our heads. Ozone is also one of the many ways that nature repairs itself when smog is present.
Ozone possesses unique properties that make it especially useful in dentistry. That’s because it’s a powerful oxidizer that we can use to very effectively kill fungi, bacteria, virus and parasites — and the concentration required is much lower than with chlorine, plus there are no toxicity issue. A single ozone molecule works as well as 3,000 to 10,000 molecules of toxic chlorine and kills pathogens thousands of times faster.
The Battle Against Oral Infections
With an ozone generator, we can take medical-grade oxygen and change it to ozone using a corona discharge reaction that works in the same way lightning generates ozone. Evidence has shown that this machine can generate the right concentration of ozone to kill many sorts of pathogens.
In dentistry, much of what we do is a fight against infections. Pathogens like bacteria, fungi and viruses cause these infections. It may be a single type of organism or several that cause the problem. These pathogens can cause other problems in the body, just as infections in other locations of the body can cause dental issues. This has been well-documented. For this and other reasons, dental infections can be difficult to completely eradicate. Infections continue to reinfect impacted areas, and this can lead to long-term dental and overall health problems.
But many pathogens share one thing in common: ozone will punch a hole in the membrane of the organism and cause it to die. In the presence of ozone, few pathogens can live. In fact, studies have shown that the body’s own antibodies create ozone in some cases to kill invading organism, but they can’t always create enough. Ozone therapy, then, is a continuation of nature’s work.
Therapeutic Goals Of Ozone Therapy
Dental ozone therapy is based on evidence-based science and meets therapeutic goals consistent with the highest standard of care. These specific goals include:
– Elimination of the pathogens
– Restoration of correct oxygen metabolism
– Establishment of a friendly ecology
– Increasing of circulation
– Activation of the immune system
– Simulation of the body’s own antioxidant system
Ozone can be applied to oral tissue through three methods for best results: ozonated water, ozonated olive oil and oxygen or ozone gas. When using ozone therapy, we use it in conjunction with other common standards of care, including x-rays, pocket-probing and clinical exams.
Two Scientific Facts Behind Dental Ozone Therapy
– Ozone is generated when energy is applied to oxygen (O2) that causes it be split into O1, then that singlet O1 molecule combines with an existing O2 molecule to create O3, also called ozone. Lightning as well as sunlight and UV light cause this to happen in nature.
– Ozone is an oxidizer or oxidant. That is, it’s a substance that accepts an electron from some other substance, called an electron acceptor. It adds an oxygen atom to a compound that is being oxidized. Healthy cells have antioxidants in their cell membranes that prohibit them from being burned up — or oxidized — by ozone. Pathogens don’t have these antioxidants or have few of them.
How Ozone Can Help You
Dentists can use ozone in the dental office to help patients in several ways, including:
Protection and prevention. Use of ozonated water on a regular basis as a pretreatment can help disinfect your mouth. Ozone disinfects and sterilizes the mouth while leaving only oxygen and water as byproducts of the process.
Treatment. For specific care purposes, ozone can be used as ozonated water or as ozone gas. These can be used for treating infections without antibiotics or chemicals — only oxygen and water. This type of treatment can be used no matter the location, size or type of infection. Gas can penetrate even deeper than water.
In Europe, ozone treatment has been used for decades to speed the healing of wounds and treat a number illnesses. Research on the topic was done as far back as the early 1900s. When used in a controlled manner, it’s safe, effective and has no side effects. That’s better than with many medications. Ozone molecules are powerful weapons that can kill microorganisms quickly and effectively without doing any damage at all to healthy human cells.
Reverse Your Cavities
Millions of patients have been treated with dental ozone, something used by dentists around the world. Yet no side effects have been recorded from using dental ozone properly. It’s possible to safely create a highly oxygenated atmosphere in the mouth that can reduce cavities and help reverse them.
And dentistry isn’t the only place where ozone is being used effectively. It’s also proving its worth at the veterinarian’s office, in the home, for skin care and in the HIV-positive community where killing viruses and bacteria is particularly important. Ozone has even shown great potential for treating diabetic foot ulcers and MRSA infections that don’t respond well to antibiotics and other treatments.
There are now hundred — perhaps thousands — of dentists in the United States who are treating patients using ozone for periodontal disease, decay therapy, remineralization, root canals, canker sores, bone infections, tooth sensitivity and much more. It is perhaps the idea of stopping and healing decay that is most unique and intriguing.
Click play, then on ‘Ozonized Water & Preventing Gum Disease From Home’
Minimally Invasive Treatment For You
In the dentist’s office, no treatment is less invasive that clean, comfortable dental ozone therapy. Early decay, in particular, can be treated effectively with ozone, preventing the need for cutting holes in teeth to remove it. We’ve managed to cut hundreds fewer holes in teeth because of minimally invasive ozone therapy.
We’ve also been amazed and astounded that this therapy can penetrate enamel and help heal and improve the deeper structure of the tooth. Few other therapies can do that. Depending on how long you’re exposed to ozone and its concentration, the penetration of the effect can be several millimeters or more.
As a dental team, there’s now a continual discussion in our office about whether to heal or whether to cut to solve a dental issue. In some cases, cutting and drilling are required, and we have the best possible array of tools to do that easily and painlessly. But sometimes, dental ozone therapy can allow us to heal your mouth instead of cutting on it. That’s an astounding advancement.
Cavities happen in an acid environment below the tooth’s surface. Ozone can kill that acid-making bacteria and effectively neutralize the waste product, creating a new environment that’s conducive to overall health and hostile to pathogens that cause disease and decay. Healthy bacteria can replace the bad ones. The acid niche is gone — and stays gone for months. With ozone treatment in the office and at home, it’s possible that the healthy situation can remain and the unhealthy situation can be kept at bay for months or years — perhaps forever.
Our ozone periodontal program includes regular oral health evaluations, cleanings, oral cancer screenings, full mouth debridement, oral hygiene coaching, ozone irrigation, ozone injections with MI desensitizer paste for total comfort and a home care kit with instructions.
Can we help you understand how ozone can be part of your dental health program? Of course, just call (619) 630-7174
Homeopathy and Dentistry
Homeopathy is a wonderfully powerful part of the medical community, and it has been often ignored by people that do not fully understand it. This article has been written to explore a little bit more about how homeopathy can really support dentistry and patients that are slightly nervous about how they are going to feel when they sit in the dentist’s chair.
One of the key things that you have to remember about homeopathy is that it address the entire body. Most forms of medicine will tend to focus on only one single part of the body: the ears, the feet, the digestives system. On the other hand, homeopathy understands that our bodies are not only made of different parts, but those parts are working together in harmony. When one part becomes unhappy and out of sync with the rest, then the rest of the body will become affected, in small ways. That means that you can feel symptoms of body unhappiness in one place, while the cause is in entirely a different place.
Normal medical doctors would focus on the place that is displaying the symptoms, and that could mean that they miss the actual cause that is upsetting the natural balance of your body. For dentists in particular, this is dramatically important. Very few people realise that our teeth can be affected by – and in turn affect –many different parts of our body; our heads, our jaws, our necks, our throat, our digestive system, even our ability to balance. A normal doctor with no understanding at all about homeopathy could very easily misdiagnose what is wrong with you, and offer you treatment that you both do not need, and could harm you.
That is why it is vitally important that your dentist has a good grounding in homeopathy, and can view you as a complete and whole human being, rather than just glaring at your gums! Here are some of the changes that a dentist can make to bring more homeopathy into their dental chair to bring a better treatment to their patients:
Arnica
Arnica has long being used for hundreds of years, because it has been proved over and over again to help people. Some of the brilliant ways that it can help a dentist’s patient is that it can reduce the feelings of shock and panic, which is essential for people that already have a fear of the dentist. It can also reduce the likelihood of nausea and gagging, which is great if a dental patient is going to have a long procedure. There is the opportunity to take a tablet full of Arnica about an hour before you go to your dentist appointment. Dentists should be making their patients aware of the amazing powers of Arnica.
Chamomilla
One of the things about going to the dentist that many people hate is the feeling of numbness that they will experience for the time after their appointment. It can be very disorientating, and really irritating if you are trying to eat! However, you simply cannot go through certain procedures at a dentists without a local anaesthetic – which you would think would put you in a difficult situation. However, there is a homeopathic remedy called Chamomilla. If you take it around fifteen minutes after your appointment has finished, it will immediately start to reduce your numbness.
 Hypericum
Hypericum
A vast amount of dental work will include upsetting your nerves, and this can be really uncomfortable and painful. However you can take some Hypericum which has been proven over and over again for encouraging nerve regrowth and healing. This is something that you can take repeatedly whilst you are healing up and recovering.
Shorter appointments
Dentists that have a good understanding of how homeopathic dentistry can really support a patient will often arrange to have short appointments with their patients. This is not because they are going to have more appointments of a shorter length, but because the changes of modern dentistry mean that it is now possible to get a lot done in a short amount of time. Many patients will find it awkward, wearying, and painful to keep their jaw locked open for a long time, and this can be very sore after a long appointment. Along with a short appointment, dentists with homeopathic knowledge will also offer Magnesium phosphorus – otherwise known as Causticum – which will relieve any cramping that a patient will feel after an appointment.
Children and dentists
Children can find going to the dentists very upsetting and difficult, but there are plenty of things that a sympathetic homeopathic dentist can do to help with this. From the very beginning, Chamomilla can be used to settle and help teething infants. No parent looks forward to teething, long nights, and crying babies, but Chamomilla can help an infant to settle down, and get the sleep that they so desperately need. As your child gets older, they may develop abscesses on their teeth which will be just as painful, and once again Chamomilla can be used to bring relief. Moving into the teenage years, braces can be very painful and sore – especially when they are tightened or moved – and Ruta can be used to help their gums and inner checks heal without extra pain.
Oral surgery
Surgery can be incredibly uncomfortable and upsetting. When we have oral or dental surgery, it can affect the way that we eat, the way that we speak, and our self-confidence. The quicker that we can heal up, the quicker we can return back to our normal lives, which is why Silica is so often recommended by dentists that understand homeopathic methods. Silica can be used twice a day for patients that really need it, and it will help with any sharp edges that are left in your mouth after surgery. However, it is very important that patients who have had an implant put into their mouth do not take Silica, as it could cause the rejection of the implant.
Bruxism
More and more people are living very stressful lives, and this has an unfortunate side effect: bruxism. Many people suffer from bruxism without even realising it, and they do not even believe that it is really a problem – but tooth clenching and grinding can actually have a very detrimental effect on your teeth. That is all bruxism is, but when people do it repeatedly, and some will do it unknowingly in their sleep, it can cause dental pain. If you are one of the many people who are struggling with bruxism, then now is the right time to talk to a dentist about this who truly appreciates homeopathic remedies.
As you can see, a normal dentist’s work can be greatly enhanced by introducing a few small changes into your dental routine. You can not only reduce pain and swelling, but also minimise any future pain and stress when you visit the dentist again. To finish off this informative article, we are going to give you some homeopathic hints and tips that you can use yourself while you are waiting to see a dentist – but remember, these are only in case you cannot see a dentist immediately. They are not complete cures:
Toothache
We have all suffered from tooth ache at one point or another, and there are many different homeopathic remedies that have been found to work that you can try out for yourself. For example, there is Belladonna. Used in huge quantities it can actually be a poison, but in very small doses it can numb the area where you are experiencing pain. You should also be aware whether your pain is hot or cold – that is, whether heat makes it worse, or cold does. Depending on what kind of pain it is, you can use Pulsatilla for hot pain, and Coffea for cold pain. If you find that clenching your teeth lessens the pain slightly, then you will find that Staphisagria will work wonders for you.
Bleeding
When a tooth has been removed from your mouth, the area can bleed much later on after the surgery. A Phosphorus tablet will work wonders here, lessening the blood flow and keepin the area clean so that it does not become infected. However, if some infection does develop then do not panic. Gunpowder – yes, you read that correctly! – actually has a wonderfully antiseptic quality. It will also reduce the pain.
Mouth ulcers
Painful and unfortunately recurring with some people, mouth ulcers can have a dramatic effect on a person’s day to day life: but with Feverfew, the patient will see their ulcers disappear easily. If you take it for a few days after the ulcers have gone, you should be prevented from any recurring attacks of ulcers, leaving your mouth pain and ulcer free.
No one likes going to the dentist, and no one likes having any changes made to their teeth – but these homeopathic ideas will naturally complement the work of a dentist. Why not call us at (619) 630-7174, and ask us about our homeopathic knowledge?
Patient Comfort Is In The Details – MI Paste
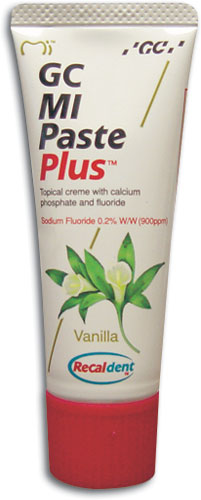 Going to the dentist can be a very stressful time – for people of all ages! That is why we do our absolute best to ensure that each and every single one of our patients is comfortable and happy with the way that their appointment goes at our dental practice. We think about each aspect of your time here, from your arrival, to your sitting in our waiting area, to seeing the dentist, to receiving any treatment or advice, to leaving us again happy and healthy. But we want to do even more than that, and look after you while you are sitting in the dentist’s chair. That is why we use MI Paste.
Going to the dentist can be a very stressful time – for people of all ages! That is why we do our absolute best to ensure that each and every single one of our patients is comfortable and happy with the way that their appointment goes at our dental practice. We think about each aspect of your time here, from your arrival, to your sitting in our waiting area, to seeing the dentist, to receiving any treatment or advice, to leaving us again happy and healthy. But we want to do even more than that, and look after you while you are sitting in the dentist’s chair. That is why we use MI Paste.
MI Paste a special protein (milk derived) that releases phosphate and calcium into your mouth, which are absolutely essential for your teeth to remain happy and healthy throughout the day. Calcium and phosphate are just two of the minerals that our teeth require to maintain themselves, but we often do not ingest enough of them in our daily diets. MI Paste also relieves tooth sensitivity, and allows Dr. Vinograd to work with your teeth with minimum pain and disruption for you. It protects the nerve endings of your teeth, thereby relieving sensitivity (not just for dentistry, but also hot/cold air and foods).. and also creating a plaque-barrier by protecting dental nerve endings. If used during each of your visits, Dr. Vinograd will be able to see a pronounced change in the way that your teeth are able to protect themselves. That could easily translate into fewer trips to the dentist for aches and pains, and fewer treatments being necessary.
We offer MI Paste at our dental clinic to ensure that you receive the best care possible, and we take pride in our ongoing efforts to ensure your comfort. MI Paste is the material favoured by holistic dental professionals to ensure that you receive the best care, and that means that our patients come to us again and again: because we take the best care of both you and your teeth.
To receive dental care that takes your comfort into consideration, make an appointment with Dr. Daniel Vinograd by calling (619) 630-7174.
Maximum Patient Comfort With New 3D Scanning Technology
Why do we use a 3d scanner at Brighon Dental San Diego? In short, for maximum comfort, precision and speed. No need for gummy impression material in your mouth. With a few passes, the wand captures the contours of your mouth, and renders a 3D model which can be sent directly to the lab via an encrypted connection.
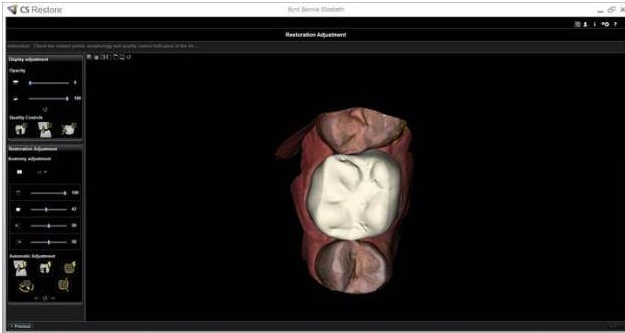
More About Our 3D Scanning Technology
The new, easy to use, and ergonomic CS 3500 intraoral scanner from Carestream Dental has a compact, lightweight design that provides a more comfortable experience for both the patient and the practitioner. Because of this design the scanner allows for high angulation scanning up to 45 degrees and depths of -2 to +13 mm. This 2D and 3D scanner has a system integration that is unique to scanning technology.
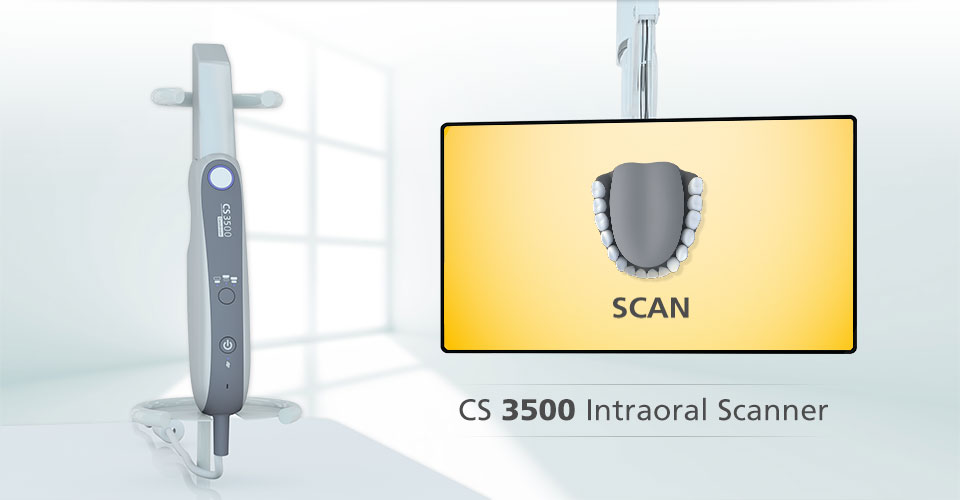
The CS 3500 can scan conventional impressions to create high precision 3D models and the technique digitizes the impressions so that crowns can easily be designed and milled. It does not require any liquids or powders to be sprayed over the teeth or gingival tissue of the patient before use. An external heater is not required because the scanner has an internal heater to prevent the mirror from becoming foggy. Also, no trolley is needed making this scanner truly portable. In addition to that, the scanner is easy for the user whether they are left handed or right handed. This scanner allows for the practitioner to spend their time focusing on their patients mouth and capturing the image rather than their computer monitor.
Capturing data with the CS 3500 is as simple as using auto focus on a phone camera. The scanner had two easy to use modes. The first is Feedback. This mode features two small but highly visible lights on the scanners body. If the light is green, the scan was good and software is building files after each acquisition. A red light means that the user is moving too much during acquisition and needs to recapture the image. This mode allows the user to focus on capturing the image and by watching the lights, a complete scan can be completed in just minutes – in most cases.
The second mode is Guide. Guide tells the user when the scanner doesn’t recognize an area, whereas Feedback waits until acquisition is captured. This mode can proactively examine the field of view to determine if the user can successfully stitch together an image. The Guide mode is best for new users.
There is a tool, Light Guidance, designed to ease use and assist in work flow which has no effect on the accuracy. It also includes True Color, a tool that can distinguish tissue and dentin/enamel if the prep is subgingival for margin definition. Executing the workflow is simple. The scanner provides multimedia commands for close-up, still, and color photos to accompany scanned data when it is exported which is something lab technicians appreciate. The doctor selects the patient from practice management software, then launches imaging software from the patients info. Scanner acquisition launches from the imaging, the user takes the scan, and saves it in the patients file. The doctor can then export the scan as an stl file from the imaging software and send it to “CS Connect” which will automatically open a web browser where the users existing labs are listed. The doctor can also write and attach notes to the case or fill out RX provided by the lab.
The scan data then moves to the lab, where the user can monitor if it’s been reviewed or not by the dashboard on the webpage. In conclusion, Carestreams’ CS 3500 intraoral scanner provides practitioners with an easy to learn, and use, highly accurate, open architecture system with a low cost port of entry. Put all of that together and you’ve found the way forward, the future of intraoral scanning technology, the game changer.
To take advantage of this 3D scanning technology, make an appointment with Dr. Daniel Vinograd by calling (619) 630-7174.
Facts about your dentures
Dentures wear out – The material used to make your dentures is very durable, but is not intended to last forever. Dentures can break if dropped and need to be replaced at regular intervals. Even with the most meticulous care, the appearance of your dentures can change with your diet, as you chew, and simply as they age. Many other factors can change the way your dentures fit in your mouth.
 Over time without teeth, gums and the bone in your jaw can shrink. If the dentures get too dry for too long, their shape may change. If the dentures are placed in hot or boiling water, they may warp, and will no longer fit properly. The gap between the denture of the gums may require the dentures to be relined. Small-diameter implants can help to protect the bone of the jaw, and keep the dentures fitting better for longer.
Over time without teeth, gums and the bone in your jaw can shrink. If the dentures get too dry for too long, their shape may change. If the dentures are placed in hot or boiling water, they may warp, and will no longer fit properly. The gap between the denture of the gums may require the dentures to be relined. Small-diameter implants can help to protect the bone of the jaw, and keep the dentures fitting better for longer.
Denture wearers need to continue regular dentist visits – If you thought losing your teeth let you off the hook in regards to visiting the dentist, think again. People who do not have teeth can still have oral problems. You should still see your dentist twice a year for an oral health assessment. Your dentist will perform an oral cancer screening, and can check for other conditions, like diabetes, that can cause symptoms in the mouth. Overtime, your jaws or your face can change, and this changes the way that your dentures fit, and your dentist can make adjustments so that they fit better. As the fit of your dentures changes, this can cause irritations, sores, or infections. Some medications, such as blood pressure medications or medication for chest pain, can have side effects, including enlargement of gum tissue, that can change the way your dentures fit. Odors, tartar, and stains will be removed by the dentist or hygienist. Your dentist will also review your medical history and any medications you may be on.
Dentures can look natural – Some people may be embarrassed by the signs of wearing a denture, such as slipping, clicking, or the worn teeth. People wearing dentures should be able to talk normally and eat without pain, or dentures falling out. Dentures can be made to look aesthetically pleasing and natural, and can even make you look younger. The red gum of the dentures can help to increase the fullness of your face, as well as supporting facial muscles, to minimize lines and wrinkles. Stability is vital for this.
You Just Got New Dentures; Now What?
While dentures are a highly effective replacement for natural teeth (and they do a great job of improving function, restoring comfort, and boosting confidence), new dentures do take some adjusting to. During the adjustment period, you may experience some trouble with the dentures. This is normal and typically lasts from one to three months, depending on your general health, condition of your mouth, your age, and the type of dentures that you wear.
Some of the most common problems that occur with new dentures include:
 Changes in your expression – It can take time for the muscles in your face, cheeks, and lips to adjust to your new dentures. Don’t be surprised if your normal expressions seem strange at first.
Changes in your expression – It can take time for the muscles in your face, cheeks, and lips to adjust to your new dentures. Don’t be surprised if your normal expressions seem strange at first.
Too much saliva – The process of digestion begins in your mouth. Anytime something new is placed in your mouth, such as food, your salivary glands begin to produce saliva. It can take days for for your saliva production to return to normal.
Soreness – The tissue in your mouth is quite sensitive and can easily become irritated by the pressure or rubbing from your new dentures. It is common for sore spots to develop. The dentures may need to be cut back in the sore areas or by the adjustments made need to be made by your dentist during follow-up visits, sometimes for weeks after receiving your new dentures.
Problems with speech – The way you speak and pronounce words is directly affected by your teeth. By their nature, dentures affect the way you talk differently from your natural teeth, and this may cause some speech difficulties. Be patient and practice. Consider reading out loud, and if you find certain words give you trouble, practice repeating them.
Difficulty chewing – Chewing may cause some discomfort in the beginning, especially until sore spots appealed.Some things you can do to make this easier include taking small bites, eating softer foods, and chewing gently. Try to chew primarily in an up-and-down motion, minimizing side to side motion in the beginning. As chewing gets easier, you can try other foods.
Kitchen sink syndrome – When you’re first getting used to your new dentures, they may make you feel like you have everything but the kitchen sink in your mouth. The new dentures feel strange in your mouth. It can take days or weeks for this feeling to subside.
Feeling loose – Until your dentures are settled all of the adjustments of been made by your dentist, the movements of your cheeks and tongue may try to dislodge her dentures. This can cause a feeling of looseness or of your dentures sliding. If you’re interested feeling loose, try closing your mouth, pressing your lips together, and gently sucking on your dentures. Before long, the dentures will settle, and the section will improve.
Gagging or nausea – New dentures may trigger a gag reflex, cause nausea and some people. This is due to the pressure of the denture on the upper palate. The dentist can make adjustments to the denture to relieve this feeling. But nausea typically dissipates within a few days.
Many of these problems can be minimized or even prevented by placing small diameter implants with the new dentures.
Denture Issues – University Study Results
Dental patients who have significant bone loss in the lower jaw, and use traditional lower dentures, frequently deal with a number of issues, including keeping them in place, trouble speaking and eating, pain from pressure points and friction, and sores due to rubbing. Dental implants placed in the lower jaw have been used with fixed bridges, hybrid denture prostheses, and removable overdentures to restore the jaws of those missing some or all of their teeth.
 Oral restoration through the use of dentures supported by two to four implants have proven to be about 96% successful. A number of studies have shown increased satisfaction in those with implant supported dentures. Meijer et al. found that patients who had implant supported dentures were significantly more satisfied with their dentures than those with complete denture treatments.
Oral restoration through the use of dentures supported by two to four implants have proven to be about 96% successful. A number of studies have shown increased satisfaction in those with implant supported dentures. Meijer et al. found that patients who had implant supported dentures were significantly more satisfied with their dentures than those with complete denture treatments.
The problem is, when patients without teeth tend to lose bone in the jaw over time. Implants require a certain amount of bone in order to be successfully placed. Insufficient bone in the jaw limits the number and length of the implants that can be placed. Placement of standard implants may require surgery to transplant bone into the jaw in order to support the implant. Elderly patients, who may have health issues or may be on anticoagulant medications, are at increased risk of surgical complications.
Smaller diameter implants that can be used to support existing dentures can now be placed without surgery. Smaller diameter implants require significantly less bone than standard implants. The procedure to place the smaller implants causes very little bleeding and much less pain. They are also less costly.
The clinical data used in this study came from an Implant Dentistry Database maintained by the New York University College of Dentistry Kriser Dental Center’s Department of Periodontology and Implant Dentistry. The data was provided without identifying information in accordance with Health Insurance Portability and Accountability Act (HIPAA) requirements. The database is certified by the Office of Quality Assurance at the University.
Satisfaction questionnaires completed by patients two months after having small diameter implant, showed that patients wore their dentures for more of the day than those with traditional dentures. The questionnaires also indicate greater patient satisfaction, with improved retention, more comfort, and lower use of denture adhesive. Patients also reported greater satisfaction with the contact between upper and lower teeth. It was also reported that the speech of those with implant supported dentures was easier to understand than those with traditional dentures. Overall, patients reported greater comfort and confidence with implants than traditional dentures.
Dentures and Dry Mouth
Sufficient saliva is important for everyone, but especially critical for denture wearers. Saliva helps to create a seal between the base of the denture and the ridge of the gums. Saliva also works to lubricate the denture and the gums to protect against irritation of the gums and prevent sores.
 In addition, dry mouth can cause dentures to fit loosely, which can lead to irritation, sores, and even infection.
In addition, dry mouth can cause dentures to fit loosely, which can lead to irritation, sores, and even infection.
There are many causes of dry mouth. Some of the most common include:
- Medications – More than 500 frequently prescribed, as well as over the counter, medications have dry mouth as a potential side effects. Medications to be wary of include blood pressure medicine, antidepressants, and decongestants.
- Illness – Some systemic conditions can inhibit the production of saliva. These conditions include chronic diarrhea, tumors of the salivary glands, liver dysfunction, and Sjogren’s Syndrome.
- Habits – Habits that cause dehydration, especially insufficient fluid intake and excessive caffeine or alcohol consumption, can all contribute to dry mouth, as can frequent mouth breathing.
- Radiation – Radiation treatment for certain cancers can lead to reduced saliva production as a side effect.
- Aging – As you get older, the salivary glands tend to produce less saliva.
Dealing with Dry Mouth
If your dry mouth is the result of prescription medication, you should talk to your doctor about alternative medications that may work without causing the dry mouth. Never stop using anything prescribed by your doctor without consulting the prescribing doctor. If an over the counter medication might be to blame, try another brand, or talk to your doctor to see what he recommends.
There are things you can do to stimulate your salivary glands. Sucking on sugar free hard candy is a simple and inexpensive way to boost the amount of saliva you have. Often, simply increasing your water consumption and reducing consumption of alcohol and caffeine can help you to be better hydrate overall, which can help your mouth tissue to be better hydrated as well. If you have a specific conditions, such as congestive heart failure or kidney disease, increasing your fluids may not be advisable, so if you have any of these conditions, talk to your doctor.
There are also mouthwashes and salivary substitutes that can be purchased from your pharmacy that can help to keep your mouth moist and improve lubrication. If all else fails, there are medications that your doctor or dentist can prescribe that can help increase your saliva production.
If you have dentures that are uncomfortable to wear because of dry mouth, consider implants. New miniature implants can help cushion your dentures and keep them securely in place.
Pros and Cons of Denture Adhesive
When a denture wearer puts their dentures in their mouth, there is a small space between the base of the denture and the gums. With brand new dentures, the space is microscopic and once the dentures are in, the space fills with saliva, creating a seal that secures the denture to the gums.
 In time, though, the bone in the jaw wears away and gum tissue changes, increasing the size of the gap and changing the way the denture fits. If you aren’t careful and you let your dentures dry out or you soak them in too hot water, they can warp, which also changes the way they fit. As the gap between gums and denture increases, the denture becomes less secure and harder to keep in place, especially the lower denture, which is easily dislodged by the tongue.
In time, though, the bone in the jaw wears away and gum tissue changes, increasing the size of the gap and changing the way the denture fits. If you aren’t careful and you let your dentures dry out or you soak them in too hot water, they can warp, which also changes the way they fit. As the gap between gums and denture increases, the denture becomes less secure and harder to keep in place, especially the lower denture, which is easily dislodged by the tongue.
Denture adhesives were created to help fill in this space and hold the denture more securely. Denture adhesives help stick the denture to the gums, which increases the suction to hold the denture in place. Many denture wearers prefer adhesive pastes to powders, as they tend to be easier to apply and less messy.
Though denture adhesive does increase retention and holds the denture more firmly in place, it can also create a false feeling of security for the wearer. Denture adhesive is really little more than a temporary solution to poorly fitting dentures that could fit better if relined or replaced.
One of the big downsides of using denture adhesive is that adhesives are messy to apply. Adhesive should be removed and the denture and mouth both thoroughly cleaned at least once a day. The sticky adhesive can be difficult and messy to remove. Add in the cost of buying the adhesives on a regular basis, and one begins to wonder if there is a better alternative.
The good news is, there is a better way. New miniature implants can be installed that will provide superior denture stability without messy, costly adhesives. The new implants are easy to place using local anesthesia, and existing dentures can be refitted to snap securely into place.
Placing implants also helps to protect the bone in the jaw and slow its erosion. Increasing stability and protecting bone will both help to minimize friction sores which are commonly caused by dentures rubbing against the gums.
Invisalign – Holistic and Modern?
Holistic medicine and dentistry is often accused of sticking to closely to the past, and to methods and techniques which frankly are outdated. This means that many people will naturally avoid those that self describe as holistic doctors or holistic dentists, because they do not believe that they will receive the optimum care that they deserve. However, this is a huge misunderstanding of exactly what the term ‘holistic’ actually means. With further study and information, it soon becomes clear that it is most definitely possible to be holistic and modern in your approach to healing the body.

This is something that Dr Vinograd really prides himself on. As well as offering the most up to date technology and procedures within his dental practice (such as Invisalign), he also keeps to his holistic principles. This means that he is able to provide his patients with centuries of holistic knowledge about the way that our bodies actually work, combined with absolutely up to date twenty first century medical procedure. Dr Vinograd is also able to offer diagnosis and treatment in just one visit, because of his years of experience within dentistry. From cosmetic dentistry, Invisalign, treatment of dental anxiety, and holistic procedures to remove pain and discomfort, there really is little that Dr Vinograd cannot offer his patients.
Dr Vinograd is a brilliant example of the holistic AND modern dentist; a man that considers each one of his patients as a whole, rather than just fixating on their teeth and gums. By following holistic rules that promote natural health, and using the finest tools and technology to rectify any problems, Dr Vinograd’s patients always know that they are in good hands when it comes to their teeth – as well as their entire health. Being holistic and modern for Dr Vinograd simply isn’t a problem.
Call (619) 630-7174 for a free Invisalign, and/or holistic dental consultation.


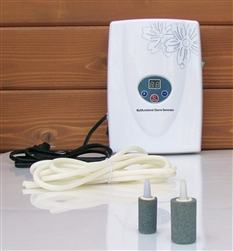 Currently, I know that a number of you have been looking for ozonizers in order to follow my protocol (for prevention of gum disease). They can be found here:
Currently, I know that a number of you have been looking for ozonizers in order to follow my protocol (for prevention of gum disease). They can be found here: 
